Advanced Fluid Management
Why Fluid Management matters
An impaired fluid status is a common condition amongst dialysis patients, and both fluid overload and fluid depletion are associated with increased mortality.1
Achieving optimal fluid status is therefore of high importance in clinical practice.
Dialysis patients may experience the probing of their individual dry weight as unpleasant, as this often provokes uncomfortable intradialytic symptoms.2
Impaired fluid status is linked to poor patient outcomes
Inadequate fluid status is harmful from these perspectives, as it is linked to poor short- and long-term patient outcomes.
The initial probing for dry weight, and thereby removing excess fluid during a dialysis session, may lead to episodes of intradialytic hypotension, cramps and dizziness.3
As quantified by data from almost 40,000 patients, over the long term, chronic fluid overload significantly increases the risk of death at all blood pressure levels.4
Chronic fluid overload and mortality in End-Stage Renal Disease (ESRD)
The original publication (graphic modified from Zoccali et al., 2017, page 2494) shows the one-year cumulative mortality risk in different categories of fluid status and pre-dialysis systolic blood pressure. Fluid-overloaded patients had a significantly higher risk of death compared with non-overloaded patients across all BP strata (all p <0.001).4
* FO – fluid overload, ** BP – blood pressure
Fluid Management solutions
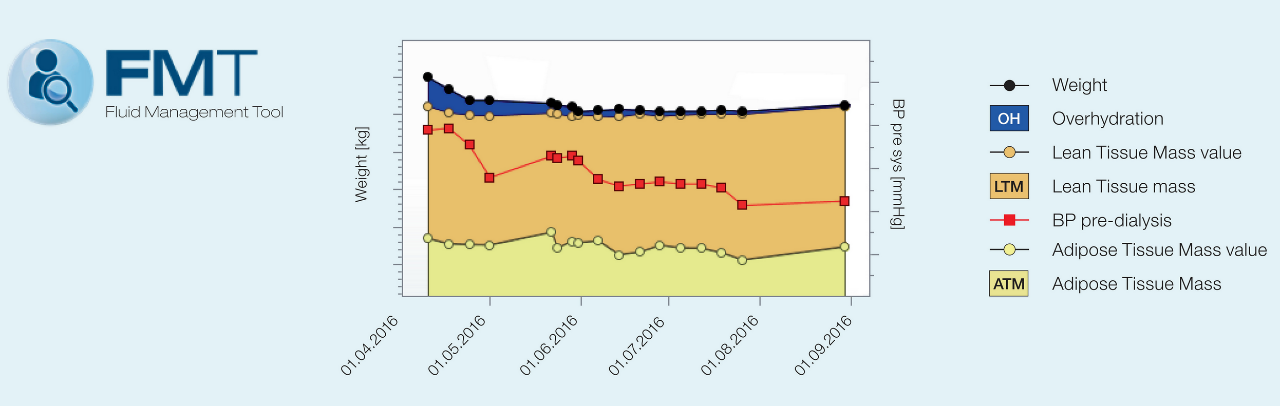
The BCM – Body Composition Monitor separates excess fluid (over-hydration) from the lean and adipose tissue components of the body on the basis of a body composition model.
This graphic is extracted from the fluid management tool and is an example which displays the chronological trend of the determined parameters.
Related content
In this section:
1 Dekker et al., Impact of fluid status and inflammation and their interaction on survival: a study in an international hemodialysis patient cohort. Kidney International (2017) 91(5): 1214-1223.
2 Agarwal et al., Dry-Weight: A Concept Revisited in an Effort to Avoid Medication-Directed Approaches for Blood Pressure Control in Hemodialysis Patients. Clin J Am Soc Nephrol (2010); 5: 1255-1260.
3 Charra, Fluid balance, dry weight, and blood pressure in dialysis. Hemodialysis International (2007), 11(1), 21-31.
4 Zoccali et al., Chronic Fluid Overload and Mortality in ESRD, J Am Soc Nephro (2017); 28(8):2496.
5 Marcelli et al., Body Composition and Survival in Dialysis Patients: Results from an International Cohort Study, Clin J Am Soc Nephrol (2015); 10(7):1192-1200.)
6 Chamney et al., A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr (2007); 85: 80-89
7 Arias-Guillén M., Bioimpedance Spectroscopy as a Practical Tool for the Early Detection and Prevention of Protein-Energy Wasting in Hemodialysis Patients. J Ren Nutr. 2018 Sep;28(5):324-332.
8 Gabrielli et al., Improved intradialytic stability during haemodialysis with blood volume-controlled ultrafiltration. J Nephrol. 2009 Mar-Apr;22(2):232-40.