Pediatric peritoneal dialysis

Less invasive therapy for a more normal life
- Bridges time to transplantation
- Easy to perform
- Less invasive than extracorporeal treatments
- Does not require anticoagulation
DISCLAIMER
Not all products and services are cleared or available for sale in all EU countries. Check your country web site for details.

Peritoneal dialysis (PD) is in general the preferred treatment modality for pediatric patients to bridge the time until transplantation1. It is easier to perform, less invasive than extracorporeal treatments and does not require anticoagulation. However, what counts most for the child and the family is that PD can be carried out at home. Fresenius Medical Care offers a comprehensive range of therapy systems adapted to the specific requirements of PD in pediatric patients:
- PD-Paed Plus
- sleep•safe harmony
- bicaVera and balance
- BCM-Body Composition Monitor
| PD-Paed Plus — PD in the smallest patients | |
|---|---|
| Easy-to-use preassembled system | PD-Paed Plus is designed to perform PD manually in premature babies, neonates and infants. It is an easy-to-use preassembled system for in-center use. |
| Flexible treatment adaptation |
|
| Safety features give confidence |
|
*Calculated on basis of a 2 exchanges per day prescription
sleep•safe harmony – Free days and protected nightime dialysis


Daily disposables do not contain PVC and DEHP*. PD bags and APD tubing set are made with Biofine.
*except APD drainage options
| Treatments tailored to young patients |
|---|
| sleep•safe harmony is a device to treat children on automated PD, in general during the night time at home. It offers high flexibility to tailor a treatment according to the individual needs of the patient: |
| Adjustable flow rates for low volume treatments |
| Special pediatric disposable set for low volumes |
| Option to perform ‘Adapted APD (aAPD)’ by varying dwell time and fill volume. |
| Giving parents the option in the treatment and its comfort |
| Integrated on-device animations guiding through the treatment procedure |
| Quiet hydraulic pump system enables a good night’s sleep |
| PIN technology reduces the number of risk steps associated with disconnection and reconnection* |
* Calculated on basis of a 4 bag connections per day prescription
bicaVera and balance — Biocompatible PD fluids
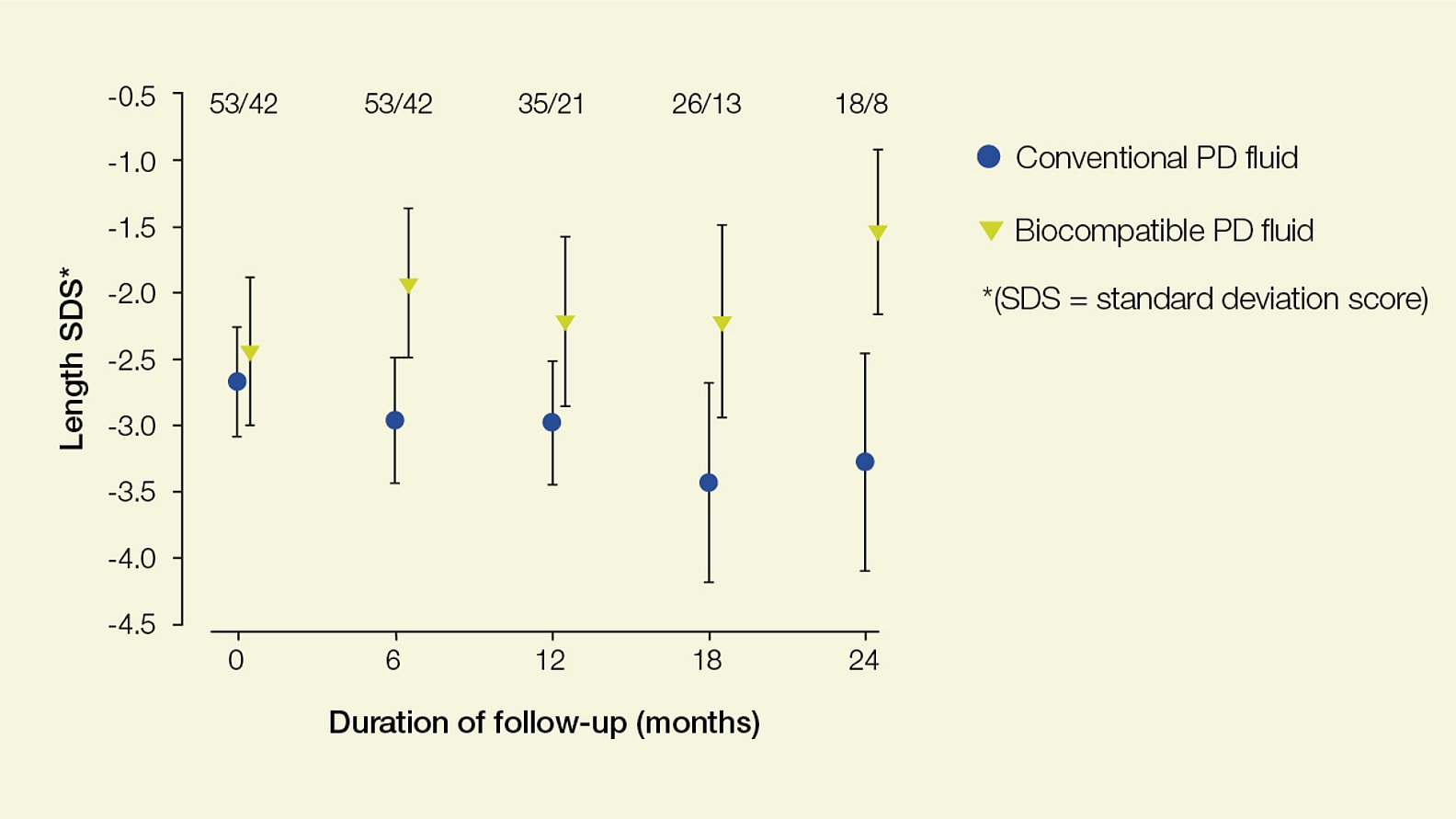
Experts recommend that biocompatible multi-chambered PD fluids which are low in glucose degradation products (GDP) should become the standard of care for children on PD2. Children dialyzed with biocom¬patible PD fluid show significant catch-up growth when compared to children on conventional solutions3.
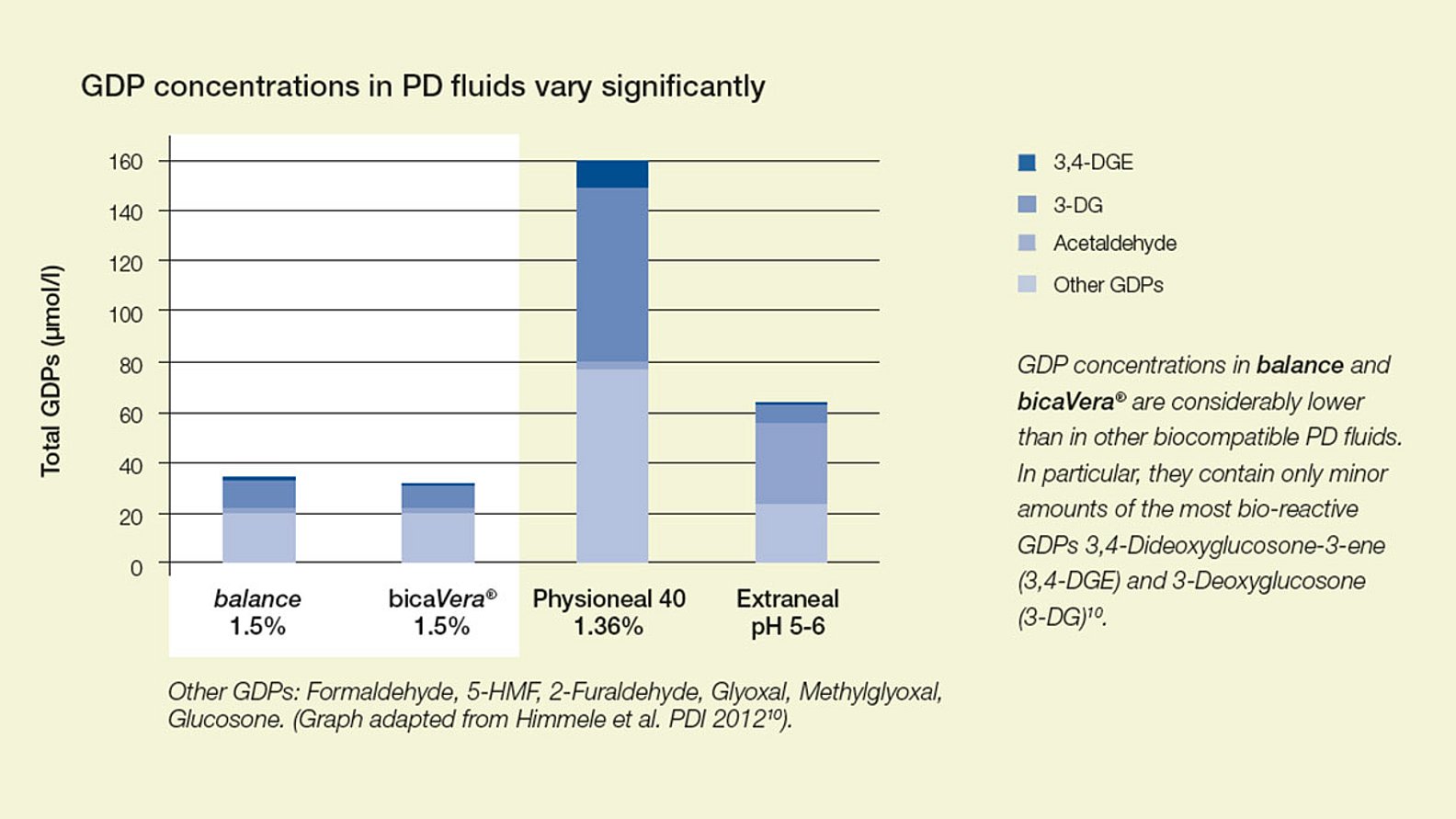
The concentration of glucose degradation products (GDPs) differs considerably. balance and bicaVera show lowest levels of GDPs compared to other biocompatible PD fluids7.
Pure bicarbonate PD fluid - bicaVera
bicaVera is purely bicarbonate-buffered and proven to better correct metabolic acidosis than lactate containing PD fluids 4,5. It is recommended in end stage renal failure2.
Less infusion pain
The use of bicarbonate-buffered PD fluids in comparison to conventional lactate-buffered fluids is associated with lower incidence of infusion pain4 and reduced capillary recruitment2.
Biocompatible fluids are essential for growth
BCM-Body Composition Monitor – Easy treatment optimization
Is the child thriving or fluid overloaded?
Especially in children on dialysis it is not always easy to differentiate between a gain in weight because of growth or because of fluid overload.
This is where the BCM-Body Composition Monitor helps you to assess the individual hydration and nutritional status of your patient. The device is based on bioimpedance spectroscopy and gives you a clear picture over time of the child’s fluid status and how the lean and fat tissue mass have developed.
- Accurate and highly reproducible data
- Based on typical pediatric reference ranges8
- Easy to apply and non-invasive
- Validated for children9,10
- Easy analysis of data with the Fluid Management Tool (FMT) on a personal computer
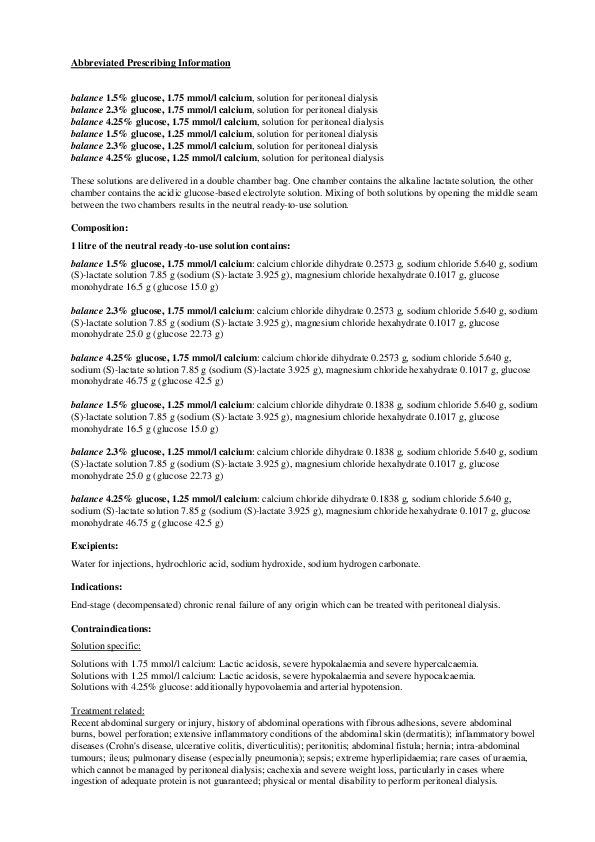
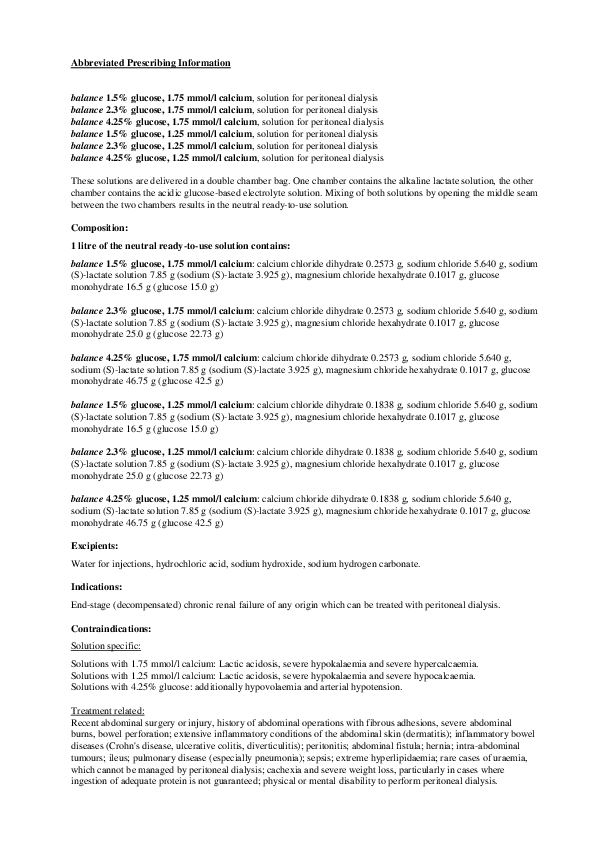
Abbreviated Prescribing Information
1 KDOQI Clinical Practice recommendations for PD adequacy. Am J Kidney Dis. 2006; 48 Suppl 1:146-158
2 Schmitt CP, Bakkaloglu SA, Klaus G, Schroeder C, Fischbach M: Solutions for peritoneal dialysis in children: recommendations by the European Pediatric Dialysis Working Group. Pediatric Nephrology 2011; 26(7):1137–47, page 1140.
3 Rees L, Azocar M, Borzych D, Watson AR, Büscher A, Edefonti A, Bilge I, Askenazi D, Leozappa G, Gonzales C, van Hoeck K, Secker D, Zurowska A, Rönnholm K, Bouts AHM, Stewart H, Ariceta G, Ranchin B, Warady BA, and Schaefer F, for the International Pediatric Peritoneal Dialysis Network (IPPN) registry. Growth in very young children undergoing chronic peritoneal dialysis. Journal of the American Society of Nephrology 2011; 22: 2303–2312, page 2307
4 Feriani M, Kirchgessner J, La Greca G, Passlick-Deetjen J. Randomized long-term evaluation of bicarbonate-buffered CAPD solution. Kidney International 1998;54(5):1731, 1732.
5 Haas S, Schmitt CP, Arbeiter K, Bonzel KE, Fischbach M, John U, Pieper AK, Schaub TP, Passlick-Deetjen J, Mehls O, Schaefer F: Improved acidosis correction and recovery of mesothelial cell mass with neutral-pH bicarbonate dialysis solution among children undergoing automated peritoneal dialysis. Journal of the American Society of Nephrology 2003;14:2632-38.
6 Mortier S, De Vriese AS, Van de Voorde J, Schaub TP, Passlick-Deetjen J, Lameire NH. Hemodynamic effects of peritoneal dialysis solutions on the rat peritoneal membrane: role of acidity, buffer choice, glucose concentration, and glucose degradation products. J Am Soc Nephrol 2002;13(2):480-9. Erratum in: Journal of the American Society of Nephrology 2002;13(5):1419-22, page 486.
7 Himmele R, Jensen L, Fenn D, Ho C, Sawin D, Diaz–Buxo J. A new neutral-pH low-GDP peritoneal dialysis fluid. Peritoneal Dialysis International 2012;32(4):449.
8 Wieskotten S, Knobloch V, Wiemann K, Wabel P, Wühl E, Schäfer F. Use of the BCM—body composition monitor in children – establishing new reference ranges. Pediatric Nephrology 2008; 23:1571–719.
9 Dasgupta I, Keane D, Lindley E, Shaheen I, Tyerman K, Schaefer F, Wühl E, Müller M, Bosy-Westphal A, Fors H, Dahlgren J, Chamney P, Wabel, P, Moissl U. Validating the use of bioimpedance spectroscopy for assessment of fluid status in children. Pediatric Nephrology (2018) 33:1601–1607.
10 Eng C, Bhowruth D, Mayes M, Stronach, L, Blaauw M, Barber A, Rees L, Shroff R. Assessing the hydration status of children with chronic kidney disease and on dialysis: a comparison of techniques. Nephrol Dial Transplant (2018) 33: 847–855.