Fresenius Medical Care offers holistic solutions for CAPD and APD patients, which includes supporting patients in preparing for PD with training solutions and the set up.
APD
Why automated peritoneal dialysis (APD)?
APD uses a programmable machine, or cycler, that controls the volume, filling, dwell time and drainage of the solution. Thanks to automated dialysis, patients can be dialyzed at home, even when sleeping.
As APD is offering more free daytime, it is the PD technique with obvious advantages for patient’s lifestyle. Patients may pursue a job and have more time for personal and family activities.1
Finally, APD cyclers offer a variety of individualization options for the treatment, allowing you to even better consider the needs of your patient, supporting you to improve patient care.
Getting started with education in APD – The difficult part was making it easier
FMC created training solutions that focus on conveying the information that really matter and offers support in preparing and setting up the treatment.
Our products - Key features of the sleep·safe harmony
sleep·safe harmony offers features aimed at improving patient care. It also provides training support by guiding on-screen animations directly on the device.
- Create prescriptions directly on the device
- On-screen keyboard
- Improved fluid usage – no extra volume for priming
- Permitted patient volume – the maximum individual fill volume
- Permitted residual volume – the maximum individual volume that may remain in the patient’s peritoneal cavity
- The goal is to:
- Reduce potential outflow alarms for a more quiet and restful sleep
- Maintain the prescribed treatment time
- Improve treatment effectiveness
- Provide more flexibility in treatment execution within defined individual limits to improve patients’ well-being and safety
- Automatic connection and barcode recognition of bags
- Integrated handles
- PatientCardplus capable of storing up to nine different prescriptions and more than 12 months of treatment data
- Automatic inline flow heating of the dialysis solution to body temperature directly during the inflow phase - no need to preheat the solution bag upfront/in advance of the treatment
- Automatic draining feature – the solution bags and the line set are drained automatically, no manual handling needed
- Plug & use – no transformer needed due to double installation
- Guiding animations directly on the device
- Large touch screen
- sleep•safe harmony system daily disposables are made of PVC-free and plasticizer-free materials such as Biofine (Except APD drainage options)
Adapted APD (aAPD) is one way to personalize treatments
sleep•safe harmony and SILENCIA offer multiple options to individualize prescriptions according to patients' needs. Using our APD cyclers, the prescription can be individualized on several levels:
- Infusion volume
- Dwell time
- Glucose profile
- Calcium profile
- FlexPoint
Different PD solutions per cycle within the same treatment can be used with sleep•safe harmony.
Because every patient is different: aAPD – Fischbach et al.2 suggests potential better results using the same time and resources2
Your patients have a chronic disease in common, but differ in many ways: age, height, weight, stage of illness, residual kidney function etc. These differences have a decision impact on the PD treatment required.
Patients’ needs are different:
Age is an important factor influencing the choice of dialysis modality. Patients with good dexterity and motivation are good candidates for PD. With increasing age, the associated comorbidities of dialysis patients might deteriorate and with it their frailty.
Management of weight is an important success factor in PD patients. Changes in weight due to lifestyle, calorie intake, disease and hydration status need constant monitoring and adaptation of PD therapy.
Dialysate to plasma ratio is a common measure used to evaluate peritoneal transport characteristic in PD patients. Patients can be into high (fast), high average and low (slow) transporters based depending upon the status of their peritoneal membrane. Peritoneal membrane transport characteristics change with time on PD. Therefore, regular monitoring of D/P creatinine and subsequent adjustment of PD prescriptions is recommended.
Patients are classified into high (fast), high average and low (slow) transporters based on the function of their peritoneal membrane. With time and increasing duration of stay on PD, patients tend to become fast transporters. PD prescriptions need to be adapted according to patients' transport status for an optimal patient outcome.
RKF has an impact on patient survival and quality of life of PD dialysis patients. Its longer preservation is a major advantage. Thus, interventions to preserve RKF, like prescription of biocompatible PD fluids, are important.
Due to compromised kidney function, bodies' own capacity to remove excess fluid also diminishes and patients need dialysis to generate UF. The amount of UF needed varies depending upon many factors, like lifestyle, disease progression and other comorbid conditions. An adequate UF is therefore critical for successful PD.
Kt/V urea is urea clearance normalized to total body water. It is an important parameter to check PD adequacy. A total Kt/V urea of at least 1.7 per week is recommended for PD patients.8
Attaining adequacy targets
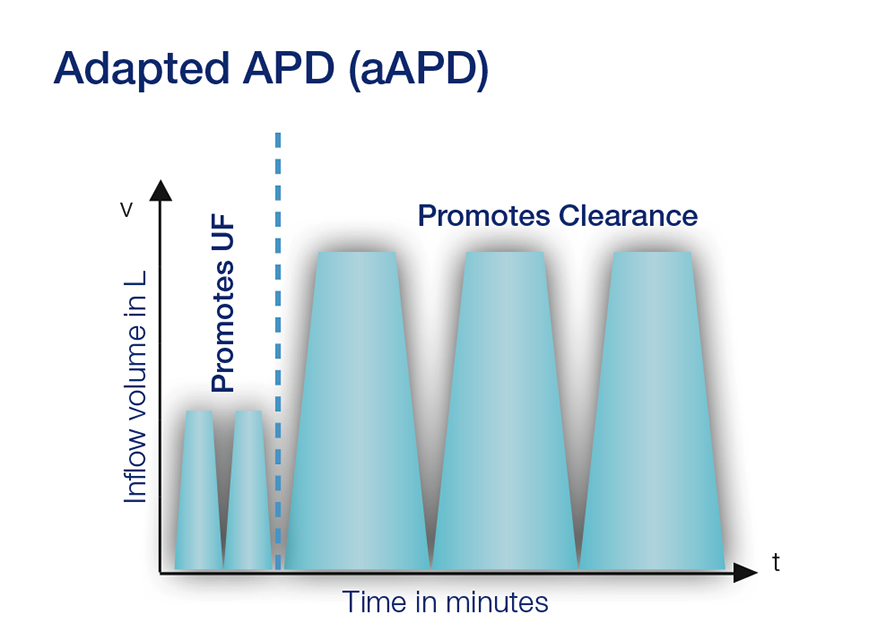
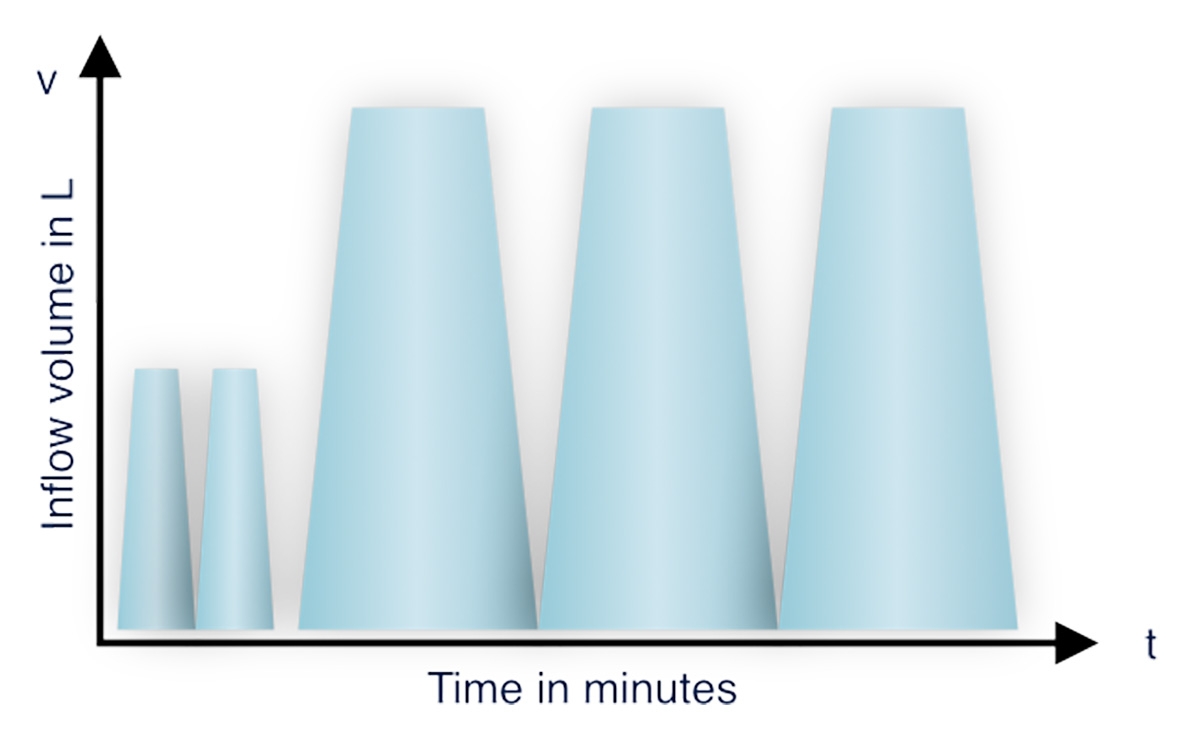
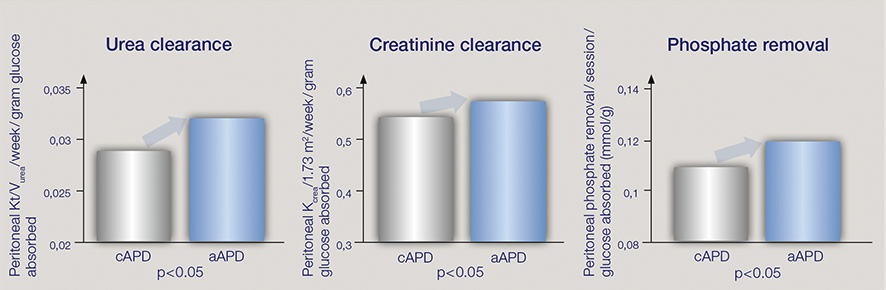
The aAPD approach was proposed by Fischbach M. et al.2 By combining sequences of short dwells and small fill volumes with long dwells and large fill volumes, aAPD aims to promote UF and clearance within one PD session. The blood purification and UF achieved for every gram of glucose absorbed was higher in aAPD in comparison to cAPD.
The challenges of PD – Reaching adequacy targets
Reaching adequacy targets in PD for both UF and clearance is challenging. Fischbach et al. propose that shorter dwell times and smaller fill volumes promote the process of UF, while longer dwell times and large fill volumes increase solute clearance.2 The proposed strategy may have the potential to improve the two targets within one PD session.
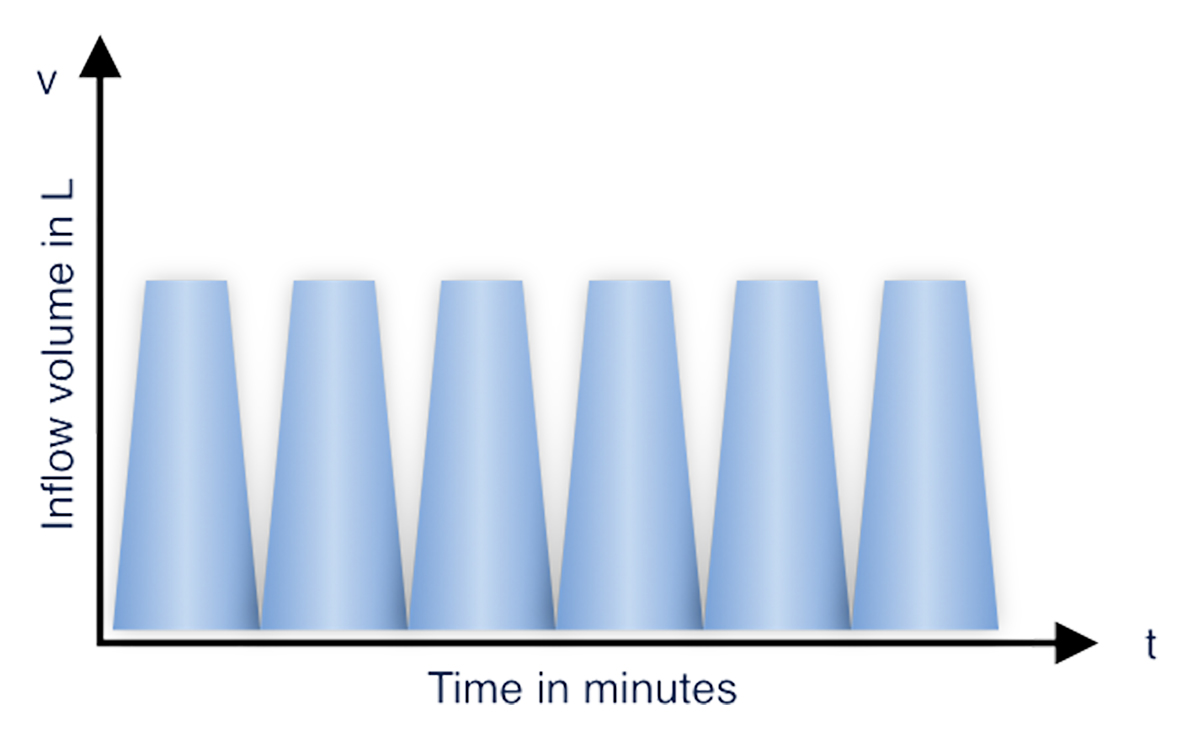
cAPD
aAPD
aAPD
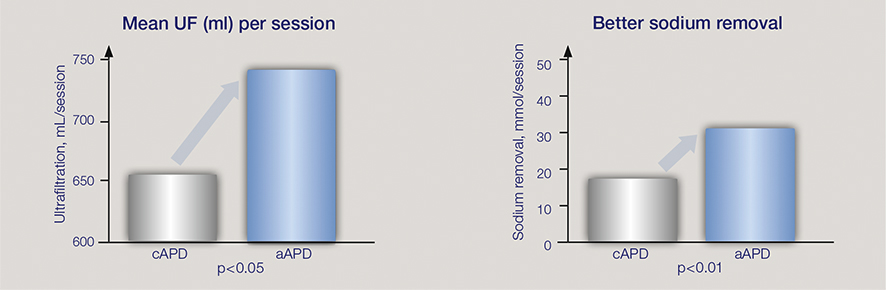
The study results suggest that, compared with cAPD, targeting UF vs. clearance separately, by varying dwell times and fill volumes may improve dialysis adequacy with a reduction in metabolic burden.2
Comparison after 45 days1
Summary of potential patient benefits as reported by Fischbach et al2
Patient benefits
- Improves ultrafiltration
- Better sodium removal
- Lower blood pressure
- Promotes clearance: urea, creatinine, phosphate
- Reduced metabolic load
Clinical value
- Improved use of existing treatment resources: better ultrafiltration and clearance with same, low glucose concentration, fluid volume and treatment time compared to cAPD
APD monitoring and support
Smart digital tools offer convenience for patients and caregivers in the comfort of the patients’ homes.
* The service is not available in all countries. The availability of the service and products must be clarified before planning or booking a vacation.
Related content
1 Roumeliotis A et al. Int Urol Nephrol 2021; 53(6):1149-1160
2 Fischbach M et al. Peritoneal Dial Int 2011; 31(4):450-458
3 Punzalan S et al. Journ of Kidn Care 2017; 2(5):262-267
4 Morales R et al. 2021 ISPD Congress, PO-40 (abstract, article submitted)
5 Unpublished data on file at Fresenius Medical Care DeutschlandGmbH; with operation noise of LAeq 12-14 dB classification as “silently operating” according to Berglund, Birgitta, Lindvall, Thomas, Schwela, Dietrich H & World Health Organization. Occupational and Environmental Health Team. (1999). Guidelines for community noise. World Health Organization, page 10, available as download under https://apps.who.int/iris/handle/10665/66217; site was accessed the last time 31/07/2023; 16:35 CET
6 Unpublished data on file at Fresenius Medical Care Deutschland GmbH (short training times)
7 Brown EA et al. Perit Dial Int. 2020;40(3):244-253.
8 Tzamaloukas AH et al. Semin Dial 2008; 21(3):250-257