Educate, coach, empower
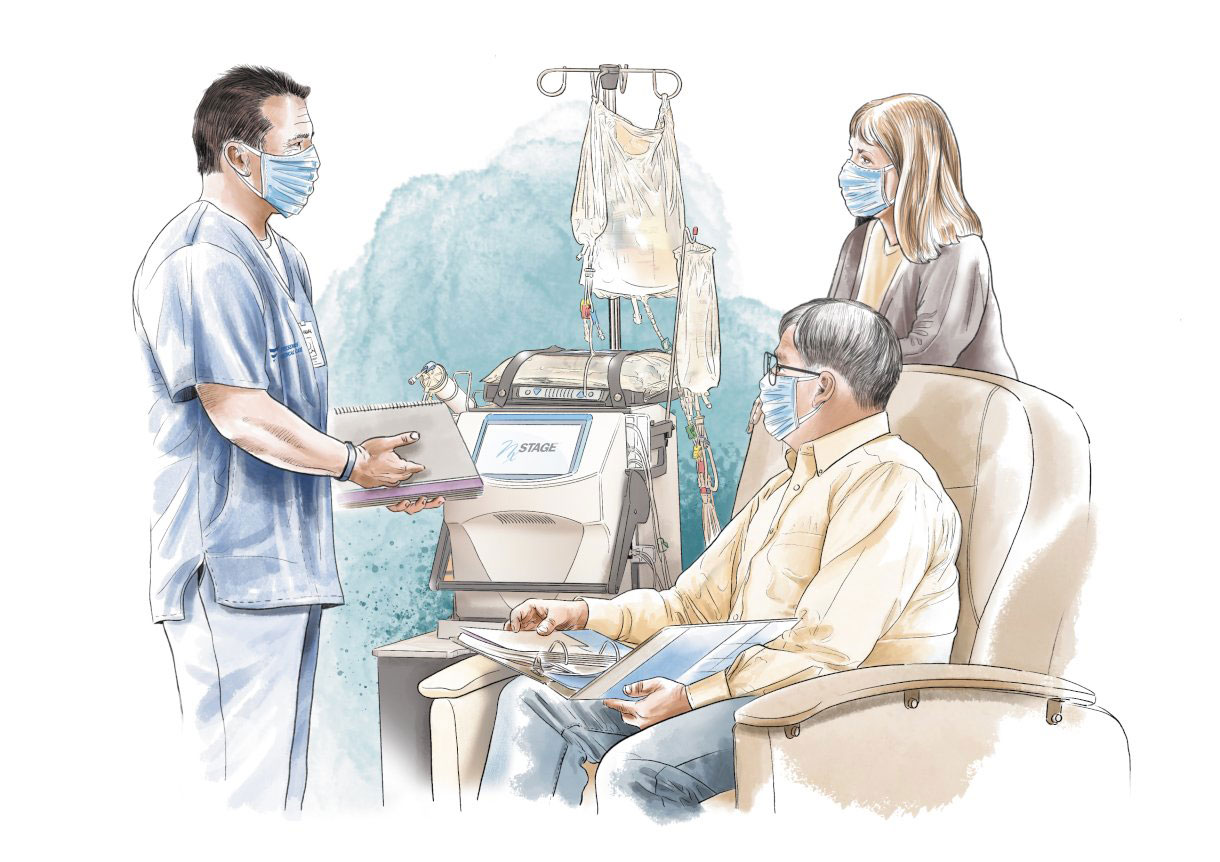
At the TCU, care givers help Vernon T. Williams to prepare for his new life.
Vernon T. Williams doesn’t believe in coincidence or chance. The retired Navy officer from Mobile, Alabama, who spent many years on a submarine, believes that everything serves a higher purpose, and that dedication and commitment will make things work out in the end. “Being on a submarine, you learn discipline and teamwork, how to deal with good and bad news, and how to react quickly to new information. You evaluate the options, make a plan and implement it,” the 71-year-old says.
This mindset helped him navigate the rough waters of a serious personal health crisis. After recurring renal cancer claimed both of his kidneys, Williams started regular dialysis treatment in the summer of 2020. He quickly discovered that the Transitional Care Units, or TCUs, created by Fresenius Medical Care North America provided him with exactly the information, attention and structure he needed to prepare for his new life. This included the choice between various treatment options. He eventually settled on and trained for home dialysis.

The care, personal training and education I received and the staff’s attention to detail was fantastic. Finding out you’re not alone gives you confidence when there’s so much to absorb and understand.
“No one in my immediate family had ever been through dialysis, so I really didn’t have a reference in terms of what to expect and what I should do,” the retired Navy officer recalls. After a first bout of kidney cancer in July 2012 that resulted in the removal of his right and partial removal of his left kidney, Williams discovered in July 2019 that the disease had returned – this time threatening the remaining left kidney. Following surgery on June 01, 2020, he had to adjust to a new world full of unknowns. “There I was, with no kidneys and lots of questions on my mind. Will I survive this? How do I learn about all the things I need to do?”
130
By the end of 2020 there were already 130 TCUs. By 2021, their number is expected to almost double to 250.
Attention to detail
His questions were answered just four days later, on June 05, when his TCU program at a Fresenius Medical Care dialysis center in Mobile began. He would spend the next month in the TCU, fully staffed with dedicated employees, whose job is to care for new dialysis patients, educate them and introduce them to the various long-term treatment options, either in-center or at home. “The care, personal training and education I received and the staff’s attention to detail was fantastic. Finding out you’re not alone gives you confidence when there’s so much to absorb and understand,” says the Navy veteran.
Williams is one of several thousand patients enrolled in a transitional care curriculum that is a fast-growing part of Fresenius Medical Care’s commitment to holistic care. TCUs were first created in the U.S. in 2018 by physicians and caregivers, who came up with the concept to address the challenges and uncertainties facing new dialysis patients. The idea resonated so well with caregivers and patients that by the end of 2020 there were already 130 TCUs. By 2021, their number is expected to almost double to 250.

The upsides of going through a TCU are better clinical outcomes, lower hospitalization rates and an improved quality of life for patients on the one hand, and higher satisfaction rates for caregivers on the other.
Starting the journey
“When we launched the first TCU in Delaware and a few other locations, we quickly realized its value. It is a great way and a wonderful opportunity to get our new patients started on their journey,” explains Melissa Herman, Senior Director Home Clinical Initiatives with Fresenius Medical Care North America. “A TCU offers us an efficient and patient-centric way to prepare our patients for the lives they will lead. And that’s why we want to expand it.”
For most new renal patients, dialysis, including visiting the center for a few hours several times a week, plus many other adjustments in terms of diet, fluid intake and general lifestyle, comes as a shock right after surgery. “Many patients who start dialysis don’t know what modalities are available to them. It’s hard to comprehend and digest so much information on top of the challenge of getting well again and coping with a new reality,” Herman explains. The trained home nurse who has worked for Fresenius Medical Care for twelve years adds: “A TCU offers patients a way to start their journey with bite-size chunks of information and more frequent dialysis sessions so they can feel better faster. And it has dedicated caregivers who can discuss their individual needs with them.”

TCUs are located within existing dialysis centers, usually in a quiet, low traffic area.
Personal relationships
A TCU is carved out of an existing dialysis center and generally comprises four dialysis stations, all in a quiet setting. It is run by a dedicated nurse and often a patient care technician, who can build a bond with their patients. They rely on a range of specialists such as social workers, insurance coordinators and dietitians to support and educate a patient with a staged curriculum that takes into account individual recovery and readiness to learn.
“These are the people who will spend four intense weeks with a patient, educating them on dialysis, fluid management and explaining the different treatment options that best fit their life,” says Herman. Patients also get the opportunity to try out or get hands-on education about different types of apparatus, from in-center equipment to a peritoneal dialysis cycler or a home hemodialysis machine, and familiarize themselves with the technology.
“The upsides of going through a TCU,” adds Herman, “are better clinical outcomes, lower hospitalization rates and an improved quality of life for patients on the one hand, and higher satisfaction rates for caregivers on the other.”

Williams completed his training and brought home a NxStage System One machine so that he could perform dialysis himself, assisted by his wife.
Getting ready for the next step
Williams came prepared, as would be expected of a Navy officer. But he still maintains that the four-week program made a big difference in getting him ready for home hemodialysis – the form of treatment he considered best suited to allow him to preserve his independence. “I like to do my homework, so I started researching and discussing the options with my wife in 2012 when I received my first cancer diagnosis. We worked out a plan, just in case.”
Back then, with the help of his nephrologist, Williams settled on home dialysis, in case he lost both kidneys, which did not happen until eight years later. “The information I received at the TCU in 2020, including going over all the available options, confirmed my previous research that home dialysis was the way to go.”
By the end of the four-week program, Williams was ready to begin training for home dialysis. “The TCU got me ready for the next step, and gave me the confidence to monitor my own treatment and understand details such as arterial and venous blood pressure. There’s a purpose behind everything you do.”
Home dialysis
In August 2020, Williams completed his training and brought home a NxStage System One machine so that he could perform dialysis himself, assisted by his wife, a registered nurse. She had traveled the world with him during his military career, making her a “tremendous and invaluable” help, as her husband puts it.
His choice of home dialysis puts him in a league with more and more renal patients who have gone through a TCU. “Around 45 percent of TCU patients choose home dialysis,” says Herman. “The number of patients who haven’t been in a TCU, but choose home dialysis treatment, is much lower, at around 15 percent.”
During the summer of 2020, fewer than one in ten new dialysis patients chose to go to a TCU, but Herman hopes that eventually at least half of all new patients will sign up. “Offering a TCU curriculum is a completely different way of doing things,” she explains. “We have to educate everyone in the market around TCUs, from admissions to the discharge planner at the hospital.”
45%
Around 45 percent of TCU patients choose home dialysis. The number of patients who haven’t been in a TCU, but choose home dialysis treatment, is much lower, at around 15 percent.
A great program awaits
Herman occasionally has patients who turn down the offer. “They feel intimidated by the whole concept at first. But after a while, they realize that our staff has a great program for getting patients involved and helping them take better control of their lives. Our goal here is to educate, coach and empower.”
Williams now has a new purpose in life – to talk about his time at the TCU with as many people as possible. “I’m a person of faith and I see this as an opportunity to reach somebody out there who is frightened. I can offer them the reassurance that there are people and technologies out there that can help them.”

